Dr. Abhimanyu Rana
Inflammatory Bowel Disease (IBD) with Pain: Navigating the Complex Path of Gastrointestinal Inflammation.
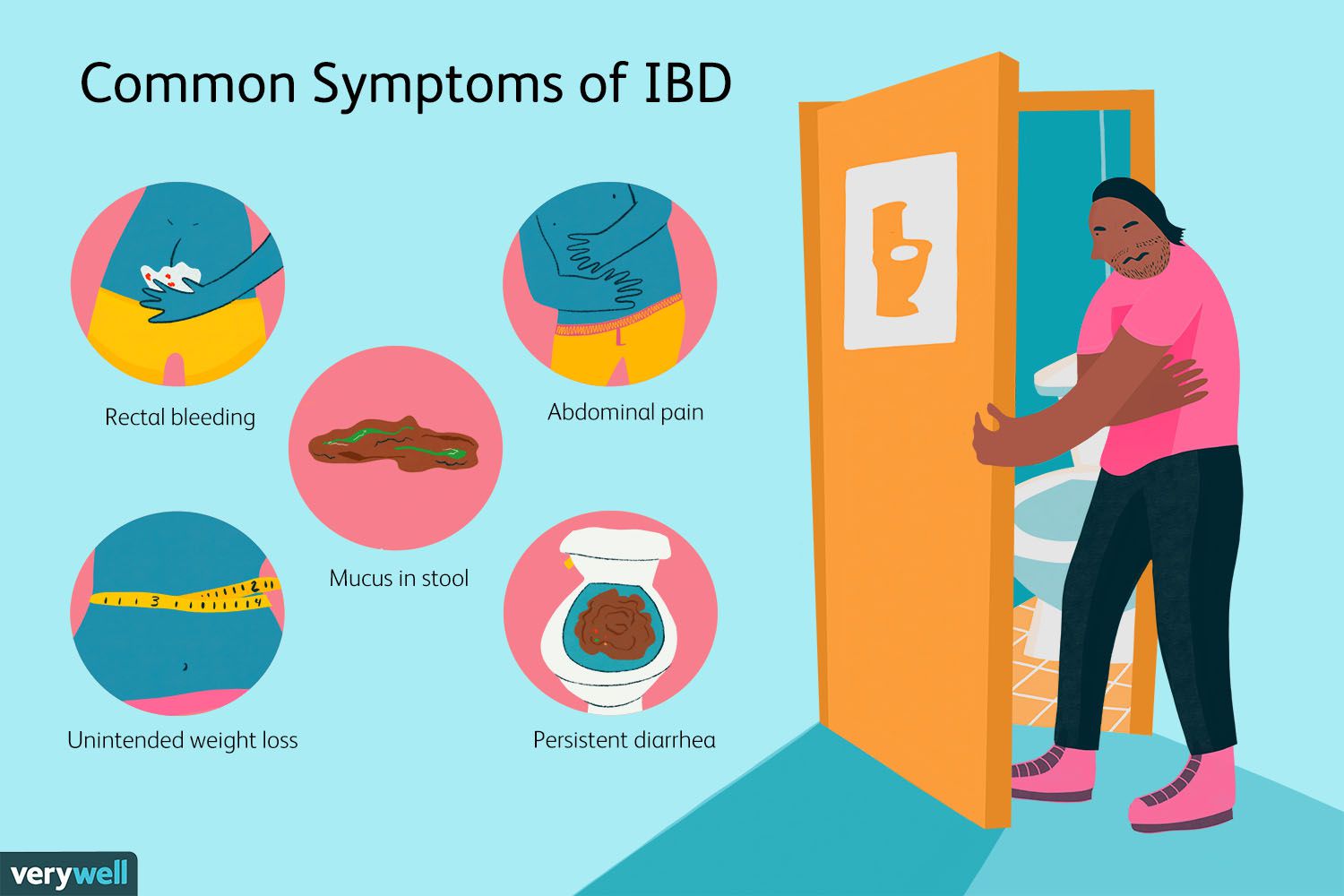
Inflammatory Bowel Disease (IBD) is a group of chronic inflammatory disorders that affect the digestive tract, leading to a range of distressing symptoms, including pain. The pain associated with IBD can significantly impact an individual's quality of life and requires a comprehensive approach to management. Understanding the multifaceted nature of IBD-related pain, its underlying mechanisms, diagnostic considerations, treatment options, and the importance of holistic care is essential for both patients and healthcare professionals.
The Landscape of IBD-Related Pain:
IBD encompasses two main conditions: Crohn's disease and ulcerative colitis. Both conditions are characterized by periods of flare-ups and remission. Pain is a common and often debilitating symptom of IBD and can manifest in various ways:
Abdominal Pain: Dull, cramp-like pain or discomfort in the abdominal region.
Localized Pain: Pain may be concentrated in specific areas of the abdomen.
Perianal Pain: Discomfort around the anus, especially in individuals with Crohn's disease.
Extraintestinal Pain: Pain may extend beyond the gastrointestinal tract, affecting joints, skin, and other organs.
Underlying Mechanisms:
The exact cause of IBD is complex and involves an interaction between genetics, immune system dysregulation, and environmental factors. Inflammation plays a central role in the development of IBD-related pain:
Immune Response: In individuals with IBD, the immune system mistakenly attacks the digestive tract, triggering chronic inflammation.
Nerve Sensitization: Ongoing inflammation can sensitize nerves in the intestines, amplifying pain signals.
Ulcers and Lesions: Ulcers, open sores, and tissue damage in the intestinal lining contribute to pain.
Muscle Contractions: Abnormal muscle contractions in the intestines can cause cramping and pain.
Holistic Approach and Patient-Centered Care:
The management of IBD-related pain extends beyond physical relief to address emotional well-being and overall quality of life. A patient-centered approach that includes open communication, collaboration with healthcare professionals, and self-care practices is essential:
Monitoring Flare-Ups: Tracking symptoms and pain patterns can help manage flare-ups effectively.
Balanced Nutrition: Adopting a balanced diet and staying hydrated can support gut health.
Stress Reduction: Engaging in stress-relief activities and practices to manage triggers.
Medication Adherence: Following prescribed treatment plans and attending regular check-ups.
Psychological Support: Seeking counseling or support groups to manage the emotional impact.

